Early Heart Attack Care (EHAC®) education promotes awareness that heart attacks have beginnings. Baptist Health works closely with the American College of Cardiology’s CardioSmart program to help educate Arkansans about better heart health.
It’s important to recognize the signs so you can take action when someone is having a heart attack. It’s also important to understand your own risk factors and symptoms so you can work with your health care provider to prevent a heart attack before it occurs.
What are the Risk Factors?
These are general risk factors for heart attack. Be sure to discuss your risk factors with your doctor.
- A family history of cardiovascular disease
- High blood pressure
- Obesity
- Sedentary lifestyle
- Use of tobacco products
- Metabolic disease, diabetes or other illnesses
- For women, it can also include use of birth control pills, a history of preeclampsia, gestational diabetes or having a low-birth-weight baby

We sat down with Ashley Mohadjer, DO, an interventional cardiologist at Baptist Health-Fort Smith to discuss top questions about early heart attack care.
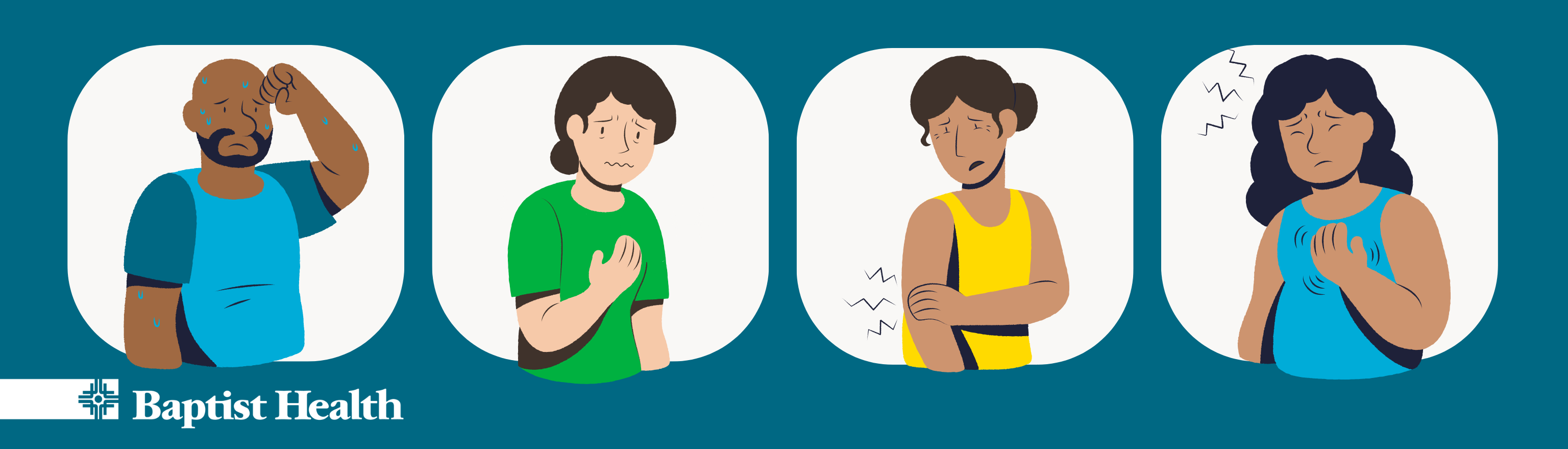
Q: What are the early signs of a heart attack that may go unnoticed?
Dr. Mohadjer: Typical signs of heart attack include chest pain, sometimes with nausea and a feeling of being clammy. Some people may have very subtle versions of these symptoms early on that seem mild. Often this may not be pain, but a very subtle discomfort in the chest that can spread up the neck and down the left arm. I have had many patients tell me that “‘it wasn’t a severe pain, so I didn’t think anything was wrong.” Other people describe this as a feeling of heartburn or indigestion that they didn’t think was heart-related until it gradually got worse prompting them to seek medical attention.
Q: How do early heart attack symptoms differ among men and women?
Dr. Mohadjer: Men typically have the textbook symptoms of a heavy, “crushing” pressure sensation in the chest that can radiate or involve the neck, jaw and left arm. This is often accompanied by a cold sweat, trouble breathing and sometimes nausea or vomiting. Women can have these symptoms as well, however, women are more likely to have different symptoms that can be more vague. In women, we often see pain or discomfort in the stomach instead of the chest. Women can also have back or shoulder discomfort that can involve the neck and sometimes both arms. Other women may have trouble breathing and significant fatigue.
Q: Are there factors or concerns women may face that men typically don’t?
Dr. Mohadjer: Emotional stress can be a trigger for heart attacks in women more so than men. Women can also suffer from heart attacks for different reasons than men altogether, which often relate to pregnancy and hormonal changes.
Q: Do some of your patients not know they’re having a heart attack?
Dr. Mohadjer: This unfortunately is not uncommon in my practice and it’s one of the reasons why I feel so strongly about health education for patients. I have had several patients realize afterward that symptoms they attributed to “acid reflux,” “overexerting myself” or even “back pain” were actually early warning signs of cardiac symptoms.
Q: How can we reduce our risk factors for a heart disease or a heart attack?
Dr. Mohadjer: Taking time to focus on prevention alone is a huge step to reduce someone’s risk for heart disease. You should get established with a primary care provider (PCP) if you don’t have one and prioritize annual wellness checks. If you have a strong family history of cardiac disease, ask your PCP to speak with a cardiologist. When it comes to diet and lifestyle changes, focus on specific and realistic goals. I tell my patients all the time that while I do want them ideally to do 30 minutes of exercise to raise their heart rates five times a week, I don’t expect this to happen overnight. If I asked anyone who doesn’t exercise regularly to run for 30 minutes tomorrow, they’d never do it again! Nobody will feel motivated to stick with a routine with that approach. Start with 5 minutes of an activity that raises your heart rate two to three times a week and hold yourself accountable for meeting that goal in a certain time frame. The next week, increase the time to 6 minutes, the following week 7 minutes, etc. Another idea is to set a distance for a brisk walk or jog, and gradually work on decreasing the amount of time it takes to accomplish that.
Survive, Don’t Drive!
One of the first things you should do if you or someone you know may be experiencing a heart attack is to call 9-1-1. Do not drive yourself or another person to the hospital in the event of a heart attack. Emergency medical service teams are trained to start life-saving treatment on the way to the hospital, minimizing damage to the heart. They can also conduct and interpret electrocardiograms to diagnose a heart attack in the ambulance and make medical personnel at the hospital aware of your condition ahead of time.
Hands-Only CPR
Hands-Only Cardiopulmonary Resuscitation (CPR) is CPR without mouth-to-mouth breaths. It can be used by people who see a teen or adult suddenly collapse in an “out of hospital” setting such as home, work or in a public place. The purpose of hands-only CPR is to get blood pumping through the victim’s body until paramedics arrive on the scene and perform more advanced life support. First, always call 9-1-1. Then push hard and fast in the center of the chest to the beat of a fast-paced song like Bee Gees’ classic disco song “Stayin’ Alive.” The song is 100 beats per minute – the minimum rate you should push on the chest during Hands-Only CPR. You can find more information and training at cpr.heart.org.