Shin splints are a common exercise-related problem with many of us experiencing them at some point. The term refers to inflammation of muscle attachments to the tibia (shin bone) on the inside of the front lower leg and usually involves small tears in the leg muscles where they are attached to the shin bone. Shin splints are characterized by pain to overexertion of the muscles. The pain usually develops gradually with dull aches after running or even walking. Small bumps and tender areas may be present along the shin bone. If untreated the pain can become more intense and potentially lead to stress fractures.
So what are the signs you can watch for and if you do experience it, what can you do about it? The physical therapists at Baptist Health Therapy Centers have put together everything you need to know about shin splints:
SIGNS AND SYMPTOMS:
- Pain or tenderness along the inside of the shin, usually the bottom half.
- Painful to touch over the shin.
- Pain is most severe at the start of a run but may dissipate during a run, as the muscles loosen up.
- May have swelling and/or redness.
CAUSES:
- Tight/Inflexible calf muscles.
- Achilles tendon tightness – places more stress onto the muscle attachments.
- Overpronation (feet flatten too much or too fast on impact).
- Excessive running on hard surfaces, such as concrete pavements.
- Biomechanically incorrect or old shoes.
- Overtraining or a rapid increase in training load or intensity.
TREATMENT:
- Rest. Stop running in the case of severe pain, if the pain is mild, then reduce the intensity of training.
- Avoid downhill running and running on uneven surfaces.
- Non-steroidal Anti-inflammatory Drugs (Ibuprofen/Naproxen).
- Local ice application.
- Massage.
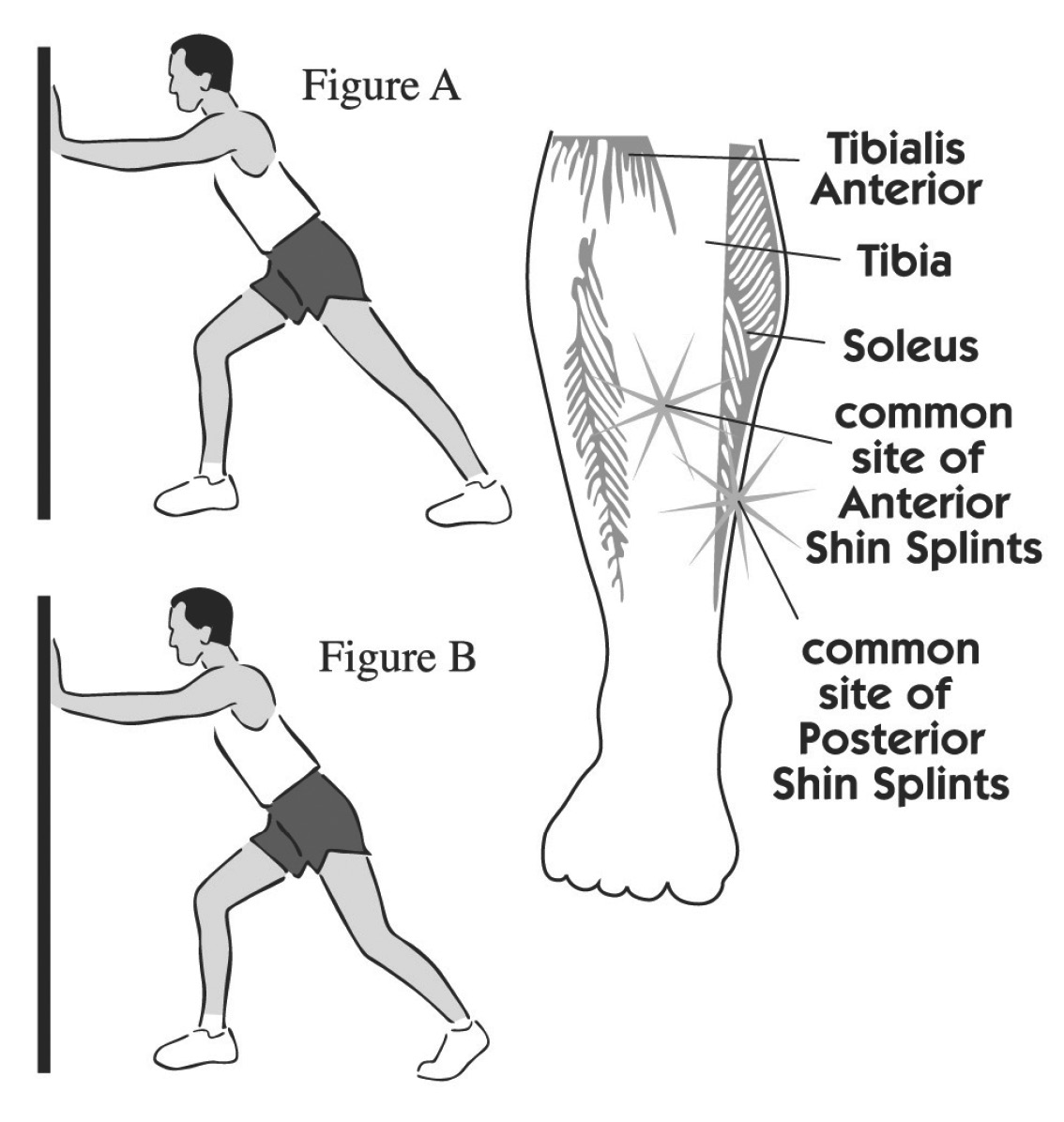
- Stretching the calf muscles (gastrocnemius and soleus muscles, see Figure A & B).
- Warm-up and stretch before running.
- Return to running gradually.
- Cross-train.
IF SELF TREATMENT FAILS:
Physical therapy may be appropriate if the injury doesn’t respond to self-treatment or a referral to an orthopaedic physician if the injury does not respond to physical therapy. A bone scan, MRI or X-ray may be necessary to check for a stress fracture.
PREVENTION:
- Stretching and warm-up of the gastrocnemius (Figure A) and soleus (Figure B) muscles. Hold each stretch for 30 seconds, relax and repeat stretches 5-6 times 3 times per day.
- Toe raises: Place a weight around the foot, and move your foot up and down from the ankle, with no movement in the rest of the leg.
- Tension band exercises. Anchor one end of an exercise band to a heavy object, such as the leg of a couch. Loop the other end around the foot. Move the foot up, down, and from side to side against the band’s resistance to exercise different muscle groups.
- Properly fit and biomechanically correct shoes for your foot type.
- Always apply ice after running.
- Run-on soft surfaces if possible.
- Avoid overstriding, which places more stress onto the shins.
- Slow sensible progression of the training program.
- Incorporate the rest of the cross-training into the training program.